How Long for Gut to Heal After Quitting Alcohol?
Understanding “how long for gut to heal after quitting alcohol” is a pivotal question, especially in the post-holiday season. In this gut health guide, Jonathan Bailor explores this question as well as explains alcohol’s effect on the gut and how to stop or at least curb alcohol intake.
Picture this: after a month of merry-making, indulging in the holiday spirit often goes hand-in-hand with a little extra indulgence in spirits of a different kind. Enter “Dry January” – a growing trend that sees many opting for an alcohol-free start to the new year. This pause in libations isn’t just a fad; it’s a step towards rejuvenating one’s overall health, starting with the gut.
Alcohol, while a staple in many holiday celebrations, doesn’t always sit well with our digestive system. Over time, it can throw off the delicate balance of our gut microbiome. But here’s the good news: giving it up, even temporarily, can initiate a remarkable healing process. The journey of the gut’s recovery from the effects of alcohol is both fascinating and crucial to understand. It’s not just about abstaining; it’s about nurturing our body back to its optimum state.
Think of the gut as a garden that needs tending. Just like a garden overrun by weeds after a storm, our gut microbiome can become imbalanced after prolonged alcohol consumption. “Dry January” is like the springtime for this inner garden, offering a chance to bloom anew. But how long does this process take? And what exactly happens inside our body when we say no to the next glass of wine?
This article dives into these intriguing questions. It’s not just a guide; it’s a journey through understanding our body’s remarkable ability to heal and thrive. Sharing this knowledge could be the key to unlocking a healthier lifestyle for someone close – a chance to show care and support for their well-being. So, as we explore the path to recovery post-alcohol, let’s remember that the journey to health is always worth sharing, especially with those we cherish.
Alcohol and Gut Health
Before we discuss how long it takes the gut to heal after quitting alcohol, we must first examine how alcohol affects the gut. It’s like understanding the extent of repairs needed in a house before commencing the renovation work. Alcohol, while often a social lubricant, can act as a disruptor in the delicate ecosystem of our gut. Let’s walk through the varied ways excessive alcohol consumption can impact gut health and the gut microbiome.
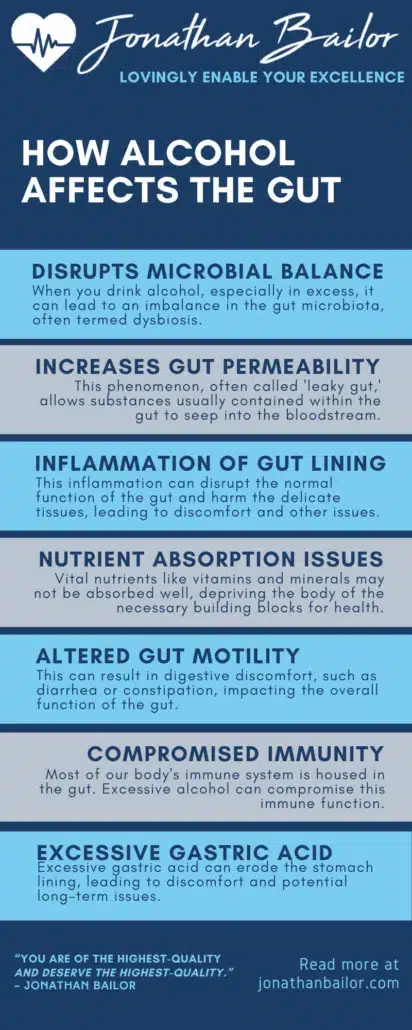
1. Disruption of Microbial Balance
Think of the human gut microbiome as a bustling city, teeming with beneficial inhabitants that keep the system running smoothly. Excessive alcohol consumption is akin to an unruly disruptor in this metropolis. When you drink alcohol, especially in excess, it can lead to an imbalance in the gut microbiota, often termed dysbiosis. This disturbance means that harmful bacteria may flourish while beneficial ones dwindle, leading to a range of digestive issues. This means that your healthy gut bacteria may not produce enough short-chain fatty acids, among other compounds, necessary for health. Imagine a city where helpful citizens are outnumbered, leading to chaos; similarly, dysbiosis can cause havoc in the gut.
2. Increased Gut Permeability
The gut lining is a vigilant gatekeeper, deciding what enters our bloodstream. Alcohol can weaken this barrier, making it more permeable. This phenomenon, often called ‘leaky gut,’ allows substances usually contained within the gut to seep into the bloodstream. This infiltration can trigger an immune response, leading to inflammation, which is akin to a security breach in a protected system. Over time, this heightened state of alert can wear down the body’s defenses.
For those dealing with alcohol-induced gut permeability and obesity-related gut issues, healthcare providers may sometimes recommend weight loss drugs for compatible individuals as part of a broader strategy to improve metabolic health. Addressing excess weight can complement efforts to restore gut integrity.
3. Inflammation and Irritation
The lining of our gut is sensitive and reacts to what we consume. Excessive alcohol can irritate this lining, leading to inflammation, much like how constant exposure to loud noise can irritate our ears. This inflammation can disrupt the normal function of the gut and harm the delicate tissues, leading to discomfort and potentially more serious conditions. It’s as if our gut walls are under constant assault, leading to wear and tear.
4. Impaired Nutrient Absorption
Our gut is a critical player in nutrient absorption. Alcohol can impair this function, leading to nutrient deficiencies. It’s akin to a malfunctioning delivery system where essential supplies don’t reach their destination. Vital nutrients like vitamins and minerals may not be adequately absorbed, depriving the body of necessary building blocks for health and well-being. Imagine a city where food supplies are disrupted, leading to a scarcity of essentials; a similar scenario can unfold in our gut.
5. Altered Gut Motility
The movement of food through our digestive system, known as gut motility, can be impacted by excessive alcohol. This effect can lead to either accelerated or slowed-down gut movement, akin to traffic being unpredictably fast or slow in a city. This irregularity can result in digestive discomfort, such as diarrhea or constipation, impacting the overall health and functionality of the gut.
6. Compromised Immune Function
Most of our body’s immune system is housed in the gut. Excessive alcohol can compromise this immune function. It’s like weakening the defenses of a fortress. The body’s ability to fight off infections and maintain health is thus impaired, making it more susceptible to illnesses. It’s as if the guardians of our health are hindered, leaving the body’s defenses lowered.
7. Contribution to Gastric Acid Production
Finally, alcohol can stimulate the production of gastric acid in the stomach. While this acid is vital for digestion, in excess, it can lead to conditions like gastritis or peptic ulcers. Imagine a cleaning substance, useful in the right amount but corrosive if overused. Excessive gastric acid can erode the stomach lining, leading to discomfort and potential long-term issues.
Understanding these impacts is the first step in recognizing the importance of giving our gut a break from alcohol. It sets the stage for exploring the healing journey that lies ahead once we decide to reduce or eliminate alcohol from our routine.
Feeling Better Is Priceless, That's Why We Don't Put A Price On It!
“It’s Like A Free and Medically Valid Version of Noom and Weight Watchers Online”
~ Dr. Doctor Matthew Oleshiak, MD
Click the 'LEARN MORE' button below for free lifetime access to the fast fix program developed by Jonathan and top Ivy League Medical Doctors
LEARN MOREP.S. It's not a free trial. It's not part of the program for free. The entire program is free, forever, for real! No credit card needed.
Health Consequences of Long-Term Alcohol Misuse: Beyond the Gut
When considering the long-term effects of alcohol dependence, also called alcohol use disorder, it’s crucial to understand the extensive range of health conditions and chronic diseases it can induce. These conditions extend beyond the gut, affecting various systems in the body. While alcohol’s impact on liver disease and cardiovascular health is widely recognized, it’s also important to highlight the specific bowel disorders and other diseases that can emerge from prolonged alcohol abuse. Let’s delve into these conditions, each revealing a facet of alcohol’s multifaceted impact on our health.
1. Irritable Bowel Syndrome (IBS)
Long-term alcohol consumption can exacerbate or even trigger Irritable Bowel Syndrome, a disorder characterized by a combination of symptoms like abdominal pain, bloating, constipation, and diarrhea. Alcohol can disrupt the normal function of the gastrointestinal tract, leading to altered gut motility and sensitivity. For individuals with IBS, alcohol can intensify symptoms, making management of the condition more challenging. It’s as if alcohol adds fuel to an already smoldering fire in the digestive system.
2. Inflammatory Bowel Diseases (IBD)
Conditions like Crohn’s disease and ulcerative colitis, which fall under the umbrella of inflammatory bowel disease, can be aggravated by chronic alcohol consumption. Alcohol can increase intestinal inflammation, exacerbate flare-ups, and even interfere with the effectiveness of medications used to treat these conditions. It’s akin to disrupting a delicate balance, where alcohol’s pro-inflammatory effects can trigger more severe and frequent bouts of IBD symptoms.
3. Gastritis and Peptic Ulcers
Chronic alcohol abuse is a well-known risk factor for gastritis and the development of peptic ulcers. Alcohol can irritate and erode the stomach’s protective lining, leading to inflammation (gastritis) or open sores (ulcers). This irritation can cause symptoms like abdominal pain, nausea, and vomiting. In severe cases, it can lead to complications like bleeding or perforation of the stomach or intestinal wall. It’s as if alcohol is slowly wearing down the protective barriers within the digestive tract.
4. Increased Cancer Risk
Prolonged alcohol use heightens the risk of various cancers, particularly those along the digestive tract, including the mouth, throat, esophagus, and colon. Alcohol acts as a carcinogen in these areas, potentially damaging cells and leading to cancerous changes. This risk is compounded by alcohol’s ability to impair the body’s natural defense mechanisms against cancer. It’s like a double-edged sword, where alcohol not only induces damage but also weakens the body’s ability to repair it.
Given this, addressing other modifiable risk factors, such as obesity, becomes even more crucial in reducing cancer risk. Managing obesity, a common risk factor for some cancers, may also involve the use of weight loss drugs for certain individuals. In such cases, reducing alcohol consumption, alongside weight management strategies, can lower the risk of digestive tract cancers and improve overall health outcomes.
5. Mental Health Disorders
The link between chronic alcohol abuse and mental health disorders like depression, anxiety, and increased stress is well-established. Alcohol can alter brain chemistry, affecting mood and cognitive function. For individuals with existing mental health issues, alcohol can exacerbate symptoms, creating a vicious cycle of worsening mental health and increased alcohol use.
6. Immune System Impairment
Regular excessive drinking episodes can weaken the immune system, increasing susceptibility to infections and slowing recovery from illnesses. Alcohol can impair the function of immune cells, making the body less capable of fighting off pathogens. This weakened state leaves the individual more prone to infections, including those that can affect the gut, like gastroenteritis.
7. Liver Disease
Chronic alcohol abuse is a leading cause of alcoholic liver disease, including fatty liver, alcoholic hepatitis, and cirrhosis. The liver, vital for detoxification and metabolism, becomes overwhelmed by excessive alcohol, leading to inflammation, scarring, and, eventually, liver failure. This progression is a stark reminder of alcohol’s toxic effects on one of the body’s crucial organs.
8. Cardiovascular Disease
While moderate alcohol consumption has been noted for potential heart benefits, heavy drinking can lead to cardiovascular problems. These include high blood pressure, cardiomyopathy, heart rhythm disorders, and increased risk of stroke. Alcohol can affect heart muscle, blood vessels, and blood pressure regulation, leading to a spectrum of heart-related issues. It’s as if the regulatory system for one of the body’s most vital organs, the heart, is thrown off balance, leading to a range of potentially serious conditions.
Understanding these health consequences highlights the importance of moderation in alcohol consumption or, in some cases, complete abstinence to preserve overall health and prevent the development or worsening of these conditions. It’s a call to action to mind our intake and listen to our body’s signals, prioritizing long-term well-being over short-term indulgence.

So, How Long for Gut to Heal After Quitting Alcohol?
The time it takes for the gut to heal after quitting alcohol varies depending on the extent of damage and individual health factors. Generally, some improvement in gut health can be noticed as early as 2-4 weeks after abstaining from alcohol. This is when the gut begins to repair its lining and restore normal gut flora.
However, complete healing and restoration of optimal gut function can take several months to a year. Factors like overall health, diet, alcohol consumption history, and supportive therapies can influence the healing process. A balanced diet rich in fiber, probiotics, and hydration, along with medical guidance, can aid in this recovery.

Lifestyle Changes to Repair and Maintain Gut Health
In the journey of healing and maintaining gut health, especially after quitting alcohol, certain lifestyle changes can play a pivotal role. Just as a garden flourishes with the right care and conditions, our gut health can significantly improve with specific, targeted lifestyle adjustments. These changes encompass not just our diet but also our overall approach to daily living. Let’s explore some of these key lifestyle modifications that can help repair the gut and foster long-term gut health.
1. Incorporate Probiotic and Prebiotic Foods
Integrating probiotic-rich foods like yogurt, kefir, and fermented vegetables can introduce beneficial bacteria to the gut. These foods aid in restoring the balance of the gut microbiome. Additionally, consuming prebiotic foods such as garlic, onions, and leafy greens can provide the necessary nutrients to support the growth of these healthy bacteria. Think of these foods as both the seeds and fertilizer needed to nurture a thriving gut garden.
2. Stay Hydrated
Hydration plays a critical role in gut health. Drinking ample water throughout the day helps maintain the mucosal lining of the intestines and facilitates digestion. It’s like ensuring a steady flow of a nurturing river that keeps the gut ecosystem balanced and functional. Aim for at least eight glasses of water daily to support gut health and overall bodily functions.
3. Manage Stress
Chronic stress can adversely affect gut health, disrupting digestive processes and exacerbating gut-related issues. Incorporating stress-reduction techniques such as meditation, yoga, or even regular walks can help. These practices are akin to creating a peaceful environment that allows the gut to function without the disruptive interference of stress.
4. Regular Physical Activity
Regular exercise can enhance gut health by improving gut motility and reducing inflammation. Activities like brisk walking, cycling, or swimming for at least 30 minutes daily can significantly contribute to a healthier gut. It’s like setting a rhythm that keeps the gut machinery running smoothly and efficiently.
5. Sleep Well
Adequate sleep is crucial for gut health. Aim for 7-8 hours of quality sleep per night to support the gut’s healing and maintenance processes. During sleep, the body undergoes repair and rejuvenation, which includes the gut. It’s as if each night is an opportunity for the gut to undergo maintenance work, ensuring it functions optimally the following day.
Adopting these lifestyle changes can create a nurturing environment for the gut to heal and maintain health. It’s about building a routine that supports the gut’s natural processes, paving the way for improved overall well-being. Remember, the path to a healthier gut is a journey that encompasses more than just dietary changes; it’s a holistic approach to living.

Safe Approaches to Quitting Alcohol
Deciding to quit drinking alcohol is a commendable step towards better health. However, it’s important to approach this change safely, especially if alcohol has been a significant part of one’s lifestyle. Quitting alcohol can be challenging, and doing it safely is crucial to avoid potential health risks associated with sudden withdrawal. Here are some effective and safe strategies to consider when deciding to quit alcohol, focusing on a gradual and supported approach to this significant lifestyle change.
1. Gradual Reduction
Instead of an abrupt halt, gradually reducing alcohol intake can help minimize withdrawal symptoms. Start by cutting back on the number of alcoholic drinks per day or week, then progressively reduce the frequency and quantity further. This method allows the body to adjust slowly to the decrease in alcohol consumption, reducing the shock to the system.
2. Seek Professional Help
Consulting with a healthcare professional or an addiction specialist can provide guidance tailored to your specific needs. They can assess your drinking patterns and offer a structured plan for quitting, which may include therapy or medication to manage withdrawal symptoms. Professional support can offer a roadmap to navigate the complexities of alcohol cessation.
3. Join Support Groups
Participating in support groups like Alcoholics Anonymous (AA) or other community support groups can provide encouragement and advice from those who have gone through similar experiences. These groups offer a sense of community and accountability, crucial in maintaining sobriety.
4. Develop Healthy Habits
Replacing drinking with healthy activities can aid in the transition. Engaging in hobbies, exercise, or other interests can provide a positive outlet and help fill the time that was previously occupied by drinking. Regular physical activity, in particular, can improve mood and reduce the urge to drink.
5. Mindfulness and Stress Management
Learning stress management techniques such as mindfulness, meditation, or yoga can help in managing cravings and emotional triggers that lead to drinking. These practices can enhance mental clarity and emotional stability, aiding in the journey towards sobriety.
6. Create a Supportive Environment
Surrounding yourself with supportive friends and family members can make a significant difference. Informing them about your decision to quit drinking can help them understand how to support you better. Additionally, avoiding environments or social settings where alcohol is a central focus can reduce temptation and help maintain your commitment to not drinking.
Quitting alcohol is a personal journey, and it’s important to find the approach that works best for you. Each step taken towards sobriety, no matter how small, is a step towards a healthier and more fulfilling life. Remember, it’s not just about eliminating a habit; it’s about creating a new, healthier lifestyle.

Frequently Asked Questions About Gut Health
Gut health is vital to overall well-being, often sparking curiosity and questions about its maintenance and impact. Here are some frequently asked questions about gut health, answered with clarity and accuracy to enhance understanding and promote a healthier lifestyle.
What is the gut microbiome, and why is it important?
The gut microbiome refers to the vast community of microorganisms residing in our digestive system, including bacteria, fungi, and viruses. This microbiome is crucial in digestion, nutrient absorption, and immune function. A balanced gut microbiome supports efficient digestion, helps produce specific vitamins, and guards against harmful pathogens. An imbalance, however, can lead to digestive issues and has been linked to various health conditions, including obesity, diabetes, and even mental health disorders.
How can diet affect gut health?
Diet is a key factor in maintaining a healthy gut. Foods rich in fiber, such as fruits, vegetables, and legumes, support the growth of beneficial gut bacteria. Probiotic foods like yogurt and kefir introduce good bacteria, while prebiotic foods like garlic and onions provide the necessary nutrients to feed these bacteria. On the other hand, a diet high in processed foods, sugar, and saturated fats can disrupt the balance of the gut microbiome, leading to digestive issues and negatively impacting overall gut health.
Can stress affect gut health?
Yes, stress can have a significant impact on gut health. Stress can alter the balance of the gut microbiome, affect gut motility, and increase gut permeability, commonly referred to as a ‘leaky gut.’ This can lead to various digestive issues, including stomach upset, bloating, and changes in bowel habits. Managing stress through relaxation techniques, adequate sleep, and regular exercise can help maintain a healthy gut.
What are the common symptoms of an unhealthy gut?
Symptoms of an unhealthy gut can vary widely but often include bloating, gas, diarrhea, constipation, and abdominal pain. Other signs might include unintentional weight changes, sleep disturbances, fatigue, skin irritations, and food intolerances. If these symptoms are persistent, it is advisable to consult a healthcare professional for proper diagnosis and treatment.
How can I improve my gut health?
Improving gut health involves a combination of dietary changes, lifestyle modifications, and stress management. A fiber-rich diet, probiotics, and prebiotics can significantly enhance gut health. Staying hydrated, engaging in regular physical activity, and ensuring adequate sleep are also important. Additionally, managing stress through mindfulness practices, meditation, or yoga can positively affect gut health.
For those whose gut health is impacted by obesity, weight loss drugs might be considered for compatible individuals in conjunction with lifestyle changes. These medications, when appropriate, can support efforts to rebalance the gut microbiome and reduce strain on the digestive system.
Understanding gut health is crucial for maintaining overall well-being. By paying attention to diet, managing stress, and adopting a healthy lifestyle, one can significantly contribute to a healthier gut and a better quality of life.
Embracing a Healthier Future: Share the Knowledge
In conclusion, navigating the path to better gut health, understanding the impact of alcohol, and adopting healthier lifestyle choices are steps towards a more vibrant life. The journey to wellness is enriched when shared. If this piece has enlightened or inspired you, consider passing this knowledge to friends and family. Sharing on social media platforms or via email can spark a positive change in someone’s life. Together, let’s spread the word about the power of making informed health decisions and their transformative effects on our well-being and that of our loved ones. Let’s embrace and share the journey to a healthier future.
Feeling Better Is Priceless, That's Why We Don't Put A Price On It!
“It’s Like A Free and Medically Valid Version of Noom and Weight Watchers Online”
~ Dr. Doctor Matthew Oleshiak, MD
Click the 'LEARN MORE' button below for free lifetime access to the fast fix program developed by Jonathan and top Ivy League Medical Doctors
LEARN MOREP.S. It's not a free trial. It's not part of the program for free. The entire program is free, forever, for real! No credit card needed.