Type 2 Diabetes: Symptoms, Causes & Natural Solutions
Type 2 Diabetes is one of the most common but preventable chronic health conditions today. In the Hormone Health Guide, Jonathan Bailor discusses the symptoms, causes, and natural solutions that may help you prevent or manage diabetes.
Navigating through the intricacies of health conditions, especially Type 2 Diabetes, can often feel like a solitary journey, particularly when seeking understanding and natural solutions. It’s a path marked by questions, concerns, and a deep yearning for a life balanced by wellness and vitality. This exploration into Type 2 Diabetes isn’t just about recognizing symptoms or identifying causes; it’s about embarking on a transformative journey towards managing blood sugar levels, aka blood glucose levels, through natural means, fostering a foundation of health and well-being that resonates with the rhythm of daily life.
Type 2 Diabetes is not just a statistic or an impersonal diagnosis; it’s a reality for many, woven into the fabric of daily decisions, from what to put on the table to how to spend a sunny afternoon. It’s about understanding how blood sugar plays a pivotal role in our well-being and discovering how to maintain healthy blood sugar levels not through restrictions but through choices that enrich life’s tapestry with vibrant hues of health.
In the heart of this exploration lies the power of knowledge—knowledge that demystifies Type 2 Diabetes and illuminates the path to managing it, not with fear but with informed, compassionate choices. It’s about uncovering the natural solutions that align with the body’s innate wisdom—solutions that are not about denying joy but about finding it in abundance through healthy harmony.
This journey is one of empowerment, a call to embrace the natural solutions that await, ready to transform the understanding of Type 2 Diabetes from a challenge to an opportunity for profound, life-enhancing change. It’s a voyage towards wellness, where every step taken is a step closer to mastering the art of living well with this disease, armed with the strength of knowledge and the power of natural solutions.
As this journey unfolds, remember that it’s not just about navigating health conditions; it’s about charting a course toward a life defined by balance, vitality, and a deep, enduring sense of well-being. Welcome to the journey towards understanding Type 2 Diabetes through the lens of symptoms, causes, and, most importantly, natural solutions that pave the way for a life embraced with health and happiness.
What is Type 2 Diabetes?
Type 2 Diabetes is a chronic health condition that unfolds in the body’s narrative over time, developing slowly, almost whispering in the background, until it becomes a chorus that can no longer be ignored. It is characterized by the body’s dance with blood sugar levels, which loses its rhythm over time. This condition emerges when the body struggles with blood sugar control, leading to a blood sugar level that is consistently higher than what is considered healthy.
At its core, Type 2 Diabetes is about the body’s relationship with glucose, the primary energy source for the cells. In a harmonious state, insulin, a hormone produced by the pancreas, escorts glucose into the cells, ensuring that blood sugar levels are balanced. However, in Type 2 Diabetes, this process becomes discordant. The cells, having been exposed to insulin’s signal too often, begin to respond with less enthusiasm, a state known as insulin resistance. Consequently, glucose lingers in the bloodstream, leading to elevated blood sugar levels.
This condition does not emerge overnight but develops slowly, tracing a path marked by subtle changes in the body’s ability to manage blood sugar. Understanding Type 2 Diabetes is the first step in rewriting the body’s approach to blood sugar control, opening the door to strategies that harmonize blood sugar levels naturally.
Navigating Through Symptoms: Understanding Type 2 Diabetes
As the journey through understanding Type 2 Diabetes continues, recognizing its common signs becomes a beacon, guiding towards early detection and management. These subtle symptoms gradually become more pronounced, echoing the body’s plea for attention and care. Each symptom tells a part of the story, revealing how elevated blood sugar levels impact the body’s intricate systems.
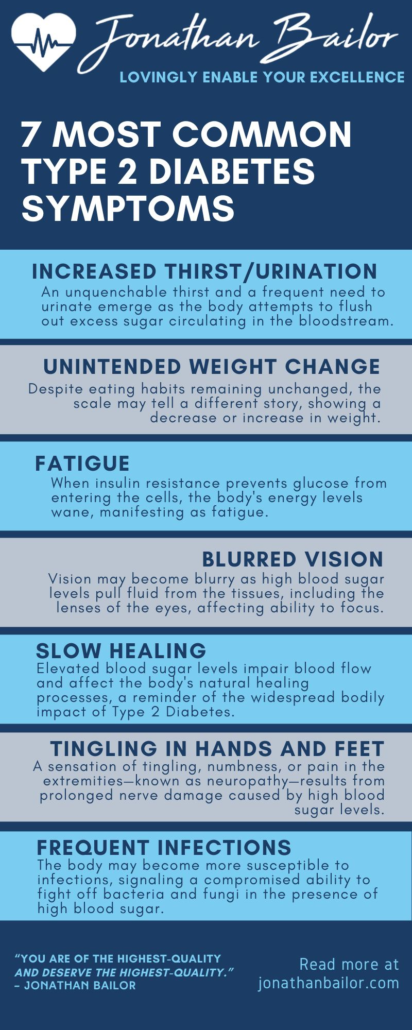
1. Increased Thirst and Frequent Urination
An unquenchable thirst and a frequent need to urinate emerge as the body attempts to flush out excess sugar circulating in the bloodstream. This symptom reflects the body’s natural inclination to seek balance, endeavoring to dilute the high blood sugar levels and expel them. However, this process also leads to a significant loss of fluids, prompting a cycle of dehydration and thirst.
2. Unintended Weight Loss or Weight Gain
Despite eating habits remaining unchanged, the scale may tell a different story, showing a decrease or increase in weight. This unexpected change is the body’s signal that glucose is not efficiently reaching the cells for energy, prompting the metabolism to burn fat and muscle for fuel instead, leading to weight loss. The excess insulin in the bloodstream can also cause weight gain.
3. Fatigue
A pervasive sense of tiredness and lack of energy characterizes this symptom, illustrating the cells’ starvation for glucose, their primary energy source. When insulin resistance prevents glucose from entering the cells, the body’s energy levels wane, manifesting as fatigue.
4. Blurred Vision
Vision may become blurry as high blood sugar levels pull fluid from the tissues, including the lenses of the eyes, affecting the ability to focus. While often reversible with blood sugar control, this symptom highlights the body’s interconnectedness and delicate balance.
5. Slow Healing of Cuts and Wounds
An observant eye might notice cuts or wounds taking longer to heal. Elevated blood sugar levels impair blood flow and affect the body’s natural healing processes, a reminder of the systemic impact of diabetes.
6. Tingling, Pain, or Numbness in the Hands or Feet
A sensation of tingling, numbness, or pain in the extremities—known as neuropathy—results from prolonged nerve damage caused by high blood sugar levels. This symptom is a critical alert to the long-term effects of unmanaged diabetes.
7. Frequent Infections
The body may become more susceptible to infections, signaling a compromised ability to fight off bacteria and fungi in the presence of high blood sugar. This symptom underscores the importance of vigilance and proactive management of blood sugar levels.
Feeling Better Is Priceless, That's Why We Don't Put A Price On It!
“It’s Like A Free and Medically Valid Version of Noom and Weight Watchers Online”
~ Dr. Doctor Matthew Oleshiak, MD
Click the 'LEARN MORE' button below for free lifetime access to the fast fix program developed by Jonathan and top Ivy League Medical Doctors
LEARN MOREP.S. It's not a free trial. It's not part of the program for free. The entire program is free, forever, for real! No credit card needed.
Unveiling the Roots: Understanding the Causes of Type 2 Diabetes
In the intricate dance of health and wellness, Type 2 Diabetes emerges, not as a sudden misstep but as the result of a complex interplay of factors, each contributes its own influence to the rhythm of blood sugar levels and insulin response. These causes, varied in their nature, share a common thread—they reflect the interconnection between lifestyle, genetics, and environmental factors, painting a picture of Type 2 Diabetes not merely as a condition but as a call to awareness and action. Exploring these causes invites a deeper understanding and opens the door to proactive lifestyle changes aimed at harmony and balance.
1. Genetic Predisposition
The tapestry of Type 2 Diabetes is often woven with threads of familial history, highlighting a genetic predisposition that predisposes individuals to the condition. While genetics set the stage, they are not the sole performers in the unfolding drama of diabetes. This intrinsic factor underscores the importance of awareness and vigilance for those with a family history, empowering them to make lifestyle choices that counterbalance this inherited risk.
2. Physical Inactivity
A sedentary lifestyle acts as a silent catalyst, gradually diminishing the body’s sensitivity to insulin. The lack of physical movement not only stagnates the body’s natural flow of energy but also hinders its ability to regulate blood sugar effectively. Regular physical activity rekindles this innate capacity, encouraging the muscles to utilize glucose and thus fostering a dynamic balance within the body’s glucose management system.
3. Excessive Weight
Carrying excessive weight, particularly around the waist, is a significant precursor to insulin resistance. The accumulation of fat, especially visceral fat, impedes insulin’s ability to function effectively, creating a barrier to the harmonious regulation of blood sugar levels. Addressing this through mindful nutrition and physical activity can dismantle the barriers, restoring fluidity and balance to insulin’s role.
4. Poor Diet
A diet saturated with highly processed foods, excessive sugars, and unhealthy fats sows the seeds of imbalance, disrupting the body’s natural rhythms of blood sugar control. This dietary pattern not only burdens the body but also dulls its sensitivity to insulin (insulin resistance), casting shadows on the landscape of health. Cultivating a diet rich in whole, nutrient-dense foods illuminates the path to balance, nurturing the body back to harmony and health.
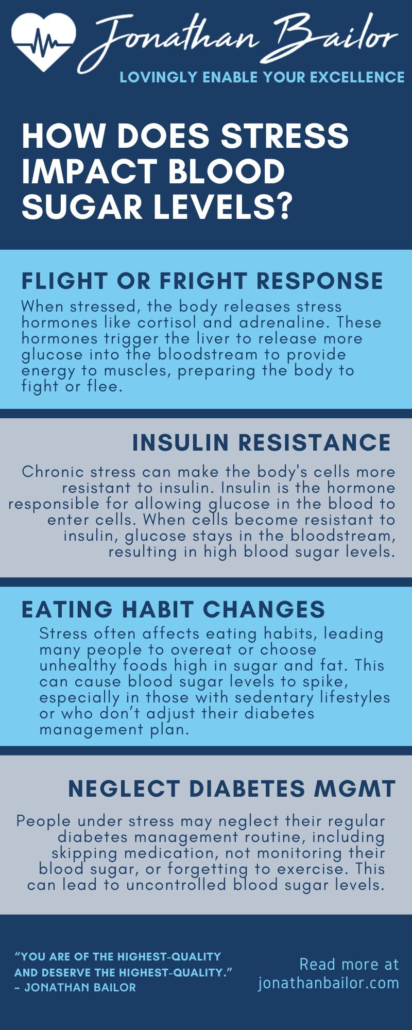
5. Stress and Hormonal Imbalances
The storms of chronic stress and resultant hormonal imbalances wreak havoc on blood sugar regulation, stirring the waters of potential diabetes onset. The release of stress hormones, such as cortisol, can elevate blood sugar levels, challenging the body’s equilibrium. Navigating through stress with practices of mindfulness, relaxation, and joy acts as a beacon of calm, guiding the body back to a haven of balance.
Understanding the causes of Type 2 Diabetes is not a conclusion but a beginning—a first step on a transformative journey toward health. It invites a reevaluation of lifestyle choices, a commitment to movement, nourishment, and peace, crafting a narrative of wellness that transcends the individual, and inspires communities and generations. In this shared journey, each step toward change is a step away from risk, a movement toward a future of health, vitality, and balance.

Understanding the Ripple Effects: Health Complications of Type 2 Diabetes
When the whispers of Type 2 Diabetes become a constant presence, the body speaks through more than just symptoms; it hints at deeper health challenges that may unfold over time. These potential diabetes complications are not mere footnotes in the narrative of diabetes management but pivotal chapters that underscore the importance of proactive, mindful engagement with one’s health. Addressing blood sugar levels and adopting lifestyle changes becomes not just an act of balancing but a profound commitment to preventing these more severe health complications.
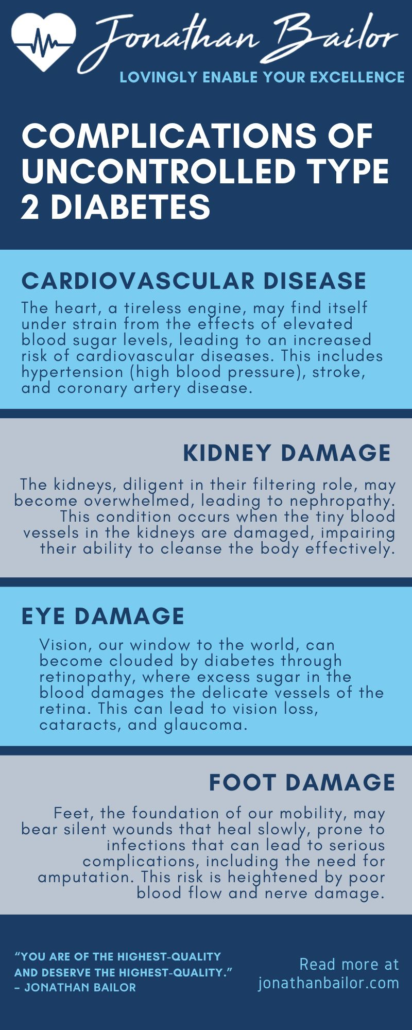
1. Cardiovascular Disease
The heart, a tireless engine, may find itself under strain from the effects of elevated blood sugar levels, leading to an increased risk of cardiovascular diseases. This includes hypertension (high blood pressure), stroke, and coronary artery disease, as high glucose levels can damage blood vessels and the nerves that control the heart, reminding us of the heart’s vulnerability and the critical importance of safeguarding it with vigilant blood sugar management.
2. Kidney Damage (Nephropathy)
The kidneys, diligent in their filtering role, may become overwhelmed, leading to nephropathy. This condition occurs when the tiny blood vessels in the kidneys are damaged, impairing their ability to cleanse the body effectively. It’s a silent reminder of the kidneys’ resilience and the need to support them through careful blood sugar control and regular monitoring.
3. Eye Damage (Retinopathy)
Vision, our window to the world, can become clouded by diabetes through retinopathy, where excess sugar in the blood damages the delicate vessels of the retina. This can lead to vision loss, cataracts, and glaucoma, highlighting the importance of regular eye exams and diligent management of blood sugar levels to preserve the gift of sight.
4. Nerve Damage (Neuropathy)
A tingling sensation, numbness, or pain in the extremities heralds neuropathy due to prolonged exposure to high blood sugar that damages the nerves. This complication not only affects physical sensation but can also impact digestion and heart function, underscoring the need for comprehensive approaches to manage blood sugar levels and protect nerve health.
5. Foot Damage
Feet, the foundation of our mobility, may bear silent wounds that heal slowly, prone to infections that can lead to serious complications, including the need for amputation. This risk is heightened by poor blood flow and nerve damage, making foot care essential to diabetes management, including regular inspection and wearing proper footwear.
6. Skin Conditions
The skin, our protective barrier, can become a canvas for bacterial and fungal infections and other skin conditions, more so for those managing diabetes. This highlights the importance of skincare, hydration, and prompt attention to any changes or breaks in the skin, ensuring its integrity and health.
Acknowledging the potential health complications of type 2 diabetes is not about casting a shadow on the journey but illuminating the path towards prevention through lifestyle changes. It’s about engaging with one’s health narrative with intention and care, crafting a daily life that supports blood sugar management, nurtures overall well-being, and fosters resilience against these complications.
Harmonizing Blood Sugar: Natural Strategies for Balance and Wellness
In the tapestry of health, maintaining balanced blood sugar levels emerges as a critical thread, weaving together the narrative of wellness and vitality. This balance is not merely about avoiding sugar or adhering to strict dietary codes; it’s about nurturing the body, mind, and spirit in ways that naturally align with the body’s rhythms and needs.
The quest to balance blood sugar levels and reduce the risk of Type 2 Diabetes is a holistic journey that encompasses nourishment, movement, rest, and mindfulness. Below are strategies that invite harmony, drawing from the wellspring of natural solutions and embodying a commitment to nurturing wellness at its core.
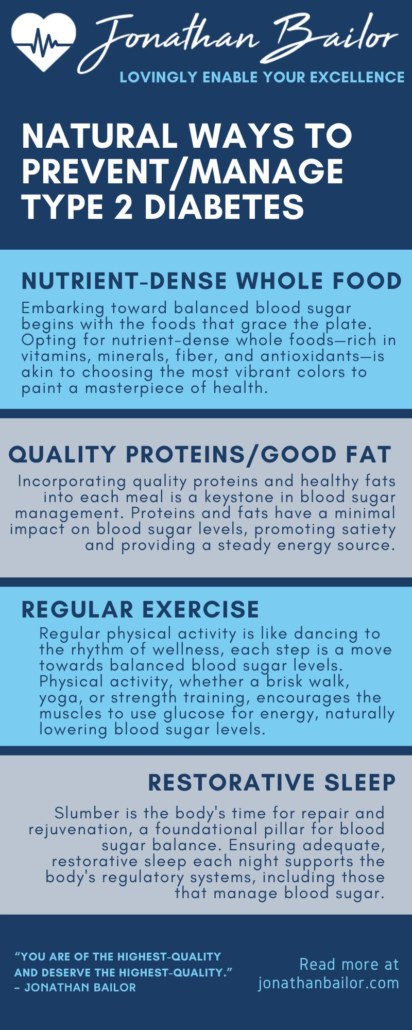
1. Embrace Nutrient-Dense Whole Foods
Embarking toward balanced blood sugar begins with the foods that grace the plate. Opting for nutrient-dense whole foods—rich in vitamins, minerals, fiber, and antioxidants—is akin to choosing the most vibrant colors to paint a masterpiece of health.
These foods, including leafy greens, non-starchy vegetables, and low-fructose fruits like berries, not only delight the palate but also support the body’s natural ability to manage glucose levels. They provide the essential nutrients that are the building blocks of wellness, nourishing the body in a way that supports blood sugar balance and overall health.
2. Prioritize Quality Proteins and Healthy Fats
Incorporating quality proteins and healthy fats into each meal is a keystone in blood sugar management. Proteins and fats have a minimal impact on blood sugar levels, promoting satiety and providing a steady energy source. Foods rich in healthy fats, such as avocados, nuts, seeds, and olive oil, along with quality proteins from sources like wild-caught fish and pasture-raised poultry, become allies in the journey toward blood sugar stability.
They play a pivotal role in crafting meals that are nourishing and sustaining, offering a steady hand to blood sugar levels.
3. Discover the Joy of Movement
Regular physical activity is like dancing to the rhythm of wellness, each step is a move towards balanced blood sugar levels. Physical activity, whether a brisk walk, yoga, or strength training, encourages the muscles to use glucose for energy, naturally lowering blood sugar levels. It’s a celebration of the body’s capabilities, enhancing insulin sensitivity and fostering a sense of vitality.
The joy of movement lies not in its intensity or duration but in its consistency and the pleasure it brings, making it a sustainable and enjoyable part of a daily routine.
4. Cultivate Mindful Eating Habits
Mindful eating transforms each meal into a moment of connection and awareness, turning attention towards the body’s cues and the experience of nourishment. It’s about savoring flavors, textures, and aromas, eating slowly, and listening to the body’s signals of hunger and fullness.
This practice encourages a harmonious relationship with food that respects the body’s needs and supports balanced blood sugar levels by preventing overeating and fostering satisfaction with meals.
5. Embrace Restorative Sleep
Slumber is the body’s time for repair and rejuvenation, a foundational pillar for blood sugar balance. Ensuring adequate, restorative sleep each night supports the body’s regulatory systems, including those that manage blood sugar.
It’s a sanctuary of rest that buffers against stress and its impact on blood sugar levels, highlighting sleep’s role not as a luxury but as a necessity for health and balance.
6. Navigate Stress with Grace
In the ebb and flow of life, stress is inevitable, but its management is a testament to resilience. Adopting stress-reduction techniques, such as meditation, deep breathing, or spending time in nature, becomes a pathway to tranquility.
These practices not only soothe the mind and spirit but also mitigate the physiological effects of stress on blood sugar levels, illustrating how peace of mind translates to peace in the body.
Balancing blood sugar levels naturally is akin to conducting a symphony of wellness, where each strategy plays a harmonious note in the grand composition of health. It’s a journey marked by mindful choices, a celebration of nourishment, movement, rest, and inner peace, each step a testament to the commitment to living vibrantly. Embracing these natural strategies opens the door to wellness, inviting balance, vitality, and a deep, enduring sense of well-being.
FAQ on Type 2 Diabetes and Hormonal Health
1. How does Type 2 Diabetes affect hormonal health?
Type 2 Diabetes intricately interacts with the body’s hormonal orchestra, playing a significant role in the overall harmony of health. Elevated blood sugar levels can lead to insulin resistance, a condition where the body’s cells become less responsive to insulin, an essential hormone regulating blood sugar. This imbalance not only disrupts the delicate equilibrium of glucose management but can also influence other hormones related to hunger, satiety, and stress, such as leptin, ghrelin, and cortisol. Understanding and managing Type 2 Diabetes is crucial to maintaining this hormonal balance, supporting the body’s natural rhythm and wellness.
2. Can balancing hormones help manage Type 2 Diabetes?
Nurturing a harmonious hormonal environment can play a pivotal role in managing Type 2 Diabetes. Individuals can positively influence their hormonal health by focusing on lifestyle choices that support insulin sensitivity and reduce insulin resistance, such as a diet rich in whole, nutrient-dense foods, regular physical activity, stress management, and adequate sleep. These actions help to stabilize blood sugar levels and improve the body’s response to insulin, highlighting the interconnectedness of hormonal health and blood sugar management.
3. What role does insulin play in Type 2 Diabetes?
Insulin serves as the maestro in the symphony of glucose management, orchestrating the movement of sugar from the bloodstream into the cells, where it’s used for energy. In Type 2 Diabetes, this process becomes discordant. The body either doesn’t produce enough insulin or becomes resistant to its effects, leading to elevated blood sugar levels. Therefore, managing insulin levels and improving insulin sensitivity are central themes in the narrative of Type 2 Diabetes care, aiming to restore balance and harmony within the body’s glucose management system.
4. Are there specific foods that support hormonal balance in Type 2 Diabetes?
While no single food can magically balance hormones, a symphony of nutrient-dense, whole foods can support hormonal health and blood sugar management. Foods rich in fiber, such as leafy greens and non-starchy vegetables, healthy fats from avocados and nuts, and quality proteins from sources like fish and legumes, contribute to a diet supporting insulin sensitivity and hormonal balance. These foods work together, much like a choir, each bringing its unique note to the harmony of health, supporting the body’s natural processes in managing Type 2 Diabetes.
5. How does stress impact blood sugar levels and hormonal health in Type 2 Diabetes?
Stress can profoundly impact blood sugar levels and hormonal health, whether it’s the ripple of daily worries or the wave of significant life events. It triggers the release of stress hormones, such as cortisol, which can increase blood sugar levels and exacerbate insulin resistance. Managing stress through mindfulness practices, relaxation techniques, and engaging in joyful activities is a counterbalance, soothing the body’s stress response. This gentle approach to stress management can support hormonal health, illustrating the power of tranquility in balancing blood sugar levels in Type 2 Diabetes.
Embarking on a Journey Together: A Call to Share
As the journey through understanding and managing Type 2 Diabetes unfolds, it becomes clear that this path is not walked alone. It’s a shared voyage, a collective endeavor that flourishes with support, understanding, and shared wisdom. By embracing the natural strategies outlined, each step is a stride towards wellness, balance, and a vibrant life.
This narrative is not just one’s own but a story to be shared with friends, family, and communities. Invite others to join this journey by sharing these insights on social media platforms and through email. Together, let’s navigate towards health, empowering one another with knowledge and unity.
Feeling Better Is Priceless, That's Why We Don't Put A Price On It!
“It’s Like A Free and Medically Valid Version of Noom and Weight Watchers Online”
~ Dr. Doctor Matthew Oleshiak, MD
Click the 'LEARN MORE' button below for free lifetime access to the fast fix program developed by Jonathan and top Ivy League Medical Doctors
LEARN MOREP.S. It's not a free trial. It's not part of the program for free. The entire program is free, forever, for real! No credit card needed.